| 5 mins read
With one in four adults now affected by mental illness, mental health problems are the largest single cause of disability in the UK. It is time for mental health to be our nation's priority, and where better to shine the spotlight than on our children?
Never before has the voice of young people been so important. Instead of being ‘seen and not heard’, they have become ‘visible with a voice’. Now we need to make sure that they are ‘partners that participate’.
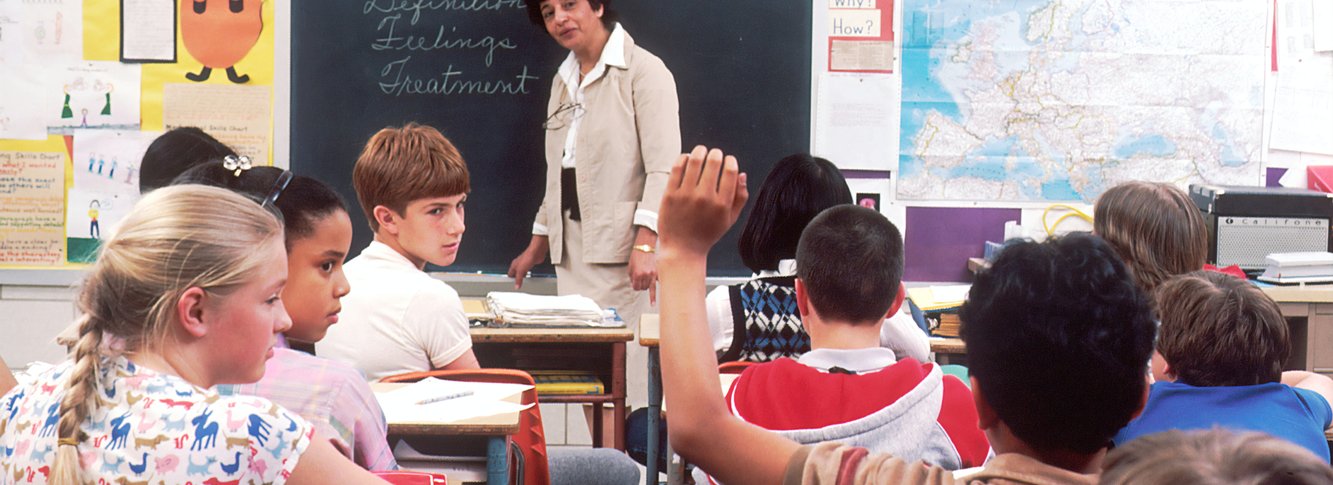
One in 10 young people have a diagnosable mental health condition – that's roughly three young people in every classroom in England. But with the NHS chronically underfunded, only a quarter of these young people are able to access the treatment and care that they so vitally need. We know that 75 per cent of all adult mental illness begins before the age of 18 years, so early intervention is not only vital, but could prevent conditions from becoming chronic, long term and disabling into adulthood.
The government has a vision, but where are the resources?
Theresa May announced plans last year to transform the way mental illness is dealt with not in our hospitals but in classrooms, at work and in our communities. The initiative has been largely welcomed, although there is concern that this is yet another governmental policy that hinges on goodwill rather than identifiable resource.
As part of this announcement, a £300m mental health plan for schools was also launched. This included incentivising every school and college in England to have a senior lead for mental health, creating new mental health support teams to liaise between schools and the NHS, and piloting a maximum four-week waiting time for children’s mental health services in some areas. The ideas are laudable but not much progress in this incentive is visible.
May should be under no illusions: she can no longer rely on the overstretched goodwill of healthcare practitioners and teachers. The landscape is not changing quickly enough – it’s time resources followed the rhetoric, or her announcements are little more than motherhood and apple pie.
Ways forward
‘Future in Mind’ (2015) and supported by ‘The 5 year Forward View for Mental Health’ (2016), provides us with an excellent blueprint for possible ways forward. It suggests ways to reconnect a disconnected system and redesign our mental health and emotional wellbeing services for young people and families through local transformation plans (LTPs) across each clinical commissioning group area in the country.
Supported by additional government investment, we must shift away from a tiered model of care to one where the whole system can meet the needs of the whole person and the whole family. We need an emphasis on building resilient communities by utilising the assets within them and the milieu of young people to develop a truly integrated service.
Moving forward, we must encourage a culture of whole system contribution to the local transformation plans. Research demonstrates that better clinical engagement means improved service quality, safety and outcomes for young people. We continue to support the importance of shared decision making with our patients in treatment and we must now support shared decision making with our clinicians in developing and delivering care. This will place value in the clinical voice alongside the skills and knowledge of our commissioners, and the views of young people and families.
Manchester devolution and the mental health revolution
Greater Manchester pioneered the industrial revolution and we believe it could pioneer our mental health revolution. With a £134 million mental health investment proposal and 60 per cent of this to support children and young people, the Greater Manchester health and social care partnership has a unique opportunity to radically transform the way we deliver and develop children and young people's mental health services. This has already been demonstrated in its first year by the success of a young people's community eating disorder network of services working in partnership with the charity BEAT.
From a 2017 green paper, Greater Manchester have also delivered a pilot schools programme to train mental health leads, and mental health first aid training to teachers and youth champions. Through the power of social prescribing and mentorship, they deliver targeted group sessions around emotional health and wellbeing whilst also connecting specialist child and adolescent mental health teams to schools to offer advice and support. Although many have challenged the ambition of this green paper, it is still a positive step forward.
For the first time, we have the opportunity work together as a whole system to build a conurbation where our children do not just survive – they thrive. After all, they are one third of our population, but all of our future.